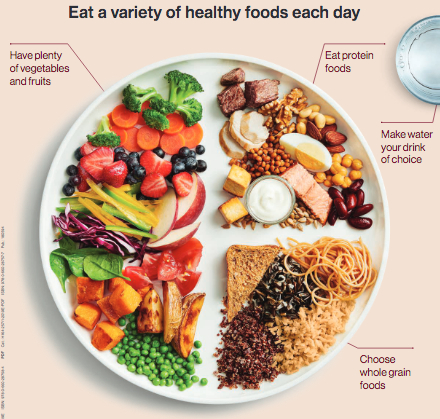
If you’re vegan, no doubt you’ve been asked that question more than once. Our protein-obsessed culture prides itself on eating tons of animals just to make sure we’re getting enough of it. But the truth is most of us are already eating way too much protein. And you don’t need meat to get it anyway! From healthy fats to calcium, plants have it all!
Just about every food contains some protein. As long as you eat a mixture of plants regularly, you’ll get plenty!
Here are the best sources of protein:
- Soy beans, tofu
- Soy milk
Great sources:
- Spinach
- Swiss chard
- Asparagus
- Bok choy
Okay, but what about iron?
We’re glad you asked! Did you know iron deficiency is no more common among vegetarians than among the general population? In fact, vegans can get enough iron by commonly eating foods that are high in iron.
You can increase your iron absorption by eating the following iron rich foods with vitamin C. This is why we put a special emphasis on cooking foods like broccoli, bok choy and tomatoes together. Also, you’ll need to keep your tea and coffee consumption away from meal times by several hours because the tannins in these drinks can make it harder to absorb iron.
Here are the best sources of iron:
- Tofu, soy milk
- Dark chocolate (+70%)
- Lentils
- Spinach, Swiss chard
- Broccoli
- Tahini/sesame seeds
- Chickpeas
- Beans (navy, kidney, lima)
- Olives
- Cumin, parsley, turmeric
Other great sources:
- Bok choy
- Asparagus
- Leeks
- Chili peppers
- Cos lettuce
What’s the deal with heme vs. non-heme iron?
While some research shows that heme (animal-based) iron is more readily absorbed by the body, other research has shown that heme iron is associated with an increased risk of heart disease, cardiovascular disease, fatal coronary heart disease and cancer. Research suggests that this may be because heme iron promotes oxidative damage and inflammation in the organs. Adding a vitamin C source to a meal increases non-heme iron absorption, making it as good as, or better than, heme iron.
Let’s talk about B12…
It can be hard to get enough vitamin B12, whatever your diet. That’s because vitamin B12 is produced by a bacteria that is removed when we wash our foods. The good news is lots of foods are fortified with B12 and you can easily get what you need by taking a supplement. If you’re concerned about your B12 intake, talk to your doctor about whether you should take a supplement.
Good sources*:
- Nutritional yeast
- Marmite
- Fortified plant milks
- Mushrooms
*If you are following a strictly plant-based diet the only reliable source of B12 is supplementation.
Healthy fats come from fish, right?
Fish are frequently cited as a good source of essential fatty acids, but the high amounts of other fats, cholesterol and toxins (like mercury) mean fish are a bad catch. Plant sources have all the benefits without putting our health on the line.
Best sources:
- Flax seeds/linseeds*
- Walnuts
- Tofu, soy milk
- Brussels sprouts
- Cauliflower
Great sources:
- Broccoli
- Cos lettuce
- Spinach, kale
- Green beans
- Strawberries, raspberries
- Bok choy, leeks, basil
*A quick note on flax seeds/linseeds – they need to be ground for your body to absorb the nutrients. Ground flax seeds can be added to a smoothie, sprinkled on cereal or on a salad.
Calcium for strong bones
The healthiest source of calcium is green leafy vegetables and legumes. People assume that milk does a body good, but research paints a different picture.
Not sure where to find plant based calcium, here are some of the best sources:
- Green leafy vegetables (e.g., spinach, bok choy)
- Tofu
- Tahini/sesame seeds
Great sources:
- Swiss chard
- Kale
- Cinnamon
Sources
Aune, D. (2017). Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality- a systematic review and dose response meta-analysis of prospective studies. International Journal of Epidemiology. 0(0), 1-27.
Food and Nutrition Board, Institute of Medicine (2002). Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids (Macronutrients). The National Academies Press, Washington.
Berk, L.S., Haddad, E.H., Hubbard, R.W, Kettering, J.D, & Peters, W.R. (1999). Dietary intake and biochemical, hematologic, and immune status of vegans compared with nonvegetarians. American Journal of Clinical Nutrition,70(suppl), 586S-93S.
Geisel, J., Herrmann, W., Hübner, U., Obeid, R., Schorr, H. (2002). The impact of vegetarianism on some haematological parameters. European Journal of Haematology, 69, 275-9.
Gleerup, A., Gramatkovski E., Rossander Hulthen, L., et al. (1995). Iron absorption from the whole diet: comparison of the effect of two different distributions of daily calcium intake. American Journal of Clinical Nutrition, 61, 97-104.
Abnet, C., Dawsey, S., Etemadi, A., Inoue-Choi, M., Graubard, B., Sinha, R., Ward, M. (2017). Mortality from different causes associated with meat, heme iron, nitrates and nitrites in the NIH-AARP Diet and Health Study: population based cohort study. British Medical Journal, 357, 1957.
Halliwell, B., Gutteridge, J.M. (1990). Role of free radicals and catalytic metal ions in human disease: An overview. Methods Enzymology, 357, 1-85.
Hallberg, L. (1981) Bioavailability of dietary iron in man. Annual Review of Nutrition, 1, 123-147.
Smith, M.V. (1988). Development of a quick reference guide to accommodate vegetarianism in diet therapy for multiple disease conditions. American Journal of Clinical Nutrition,48, 906-909.
Kwak, S.M., Lee, J., Myung, S.K. (2012). Efficacy of omega-3 fatty acid supplements (eicosapentaenoic acid and docosahexaenoic acid) in the secondary prevention of cardiovascular disease: a meta-analysis of randomized, double-blind, placebo-controlled trials. Archives of Internal Medicine; 172, 986-994.
Khaw, K.T., Lentjes, M.A.H., Shakya-Shrestha, S., Wareham, N.J., & Welch, A.A. (2010) Dietary intake and status of n-3 polyunsaturated fatty acids in a population of fish-eating and non-fish-eating meat-eaters, vegetarians, and vegans and the precursor-product ratio of a-linolenic acid to long-chain n-3 polyunsaturated fatty acids: results from the EPIC-Norfolk cohort. American Journal of Clinical Nutrition, 92, 1040-1051.
Barnard, N.D., Berkow, S.E., Lanou, A.J. (1988) Calcium, dairy products and bone health in children and young adults: a re-evaluation of evidence. Pediatrics, Mar; 115(3), 736-43.
Gordon, C.M., Kocher, M.S., Sonneville, K.R. (2012). Vitamin D, calcium and dairy intakes and stress fractures among female adolescents. Archives of Pediatric Adolescent Medicine, Jul 1; 166(7), 595-600.
Feskanich, D. (2003). Calcium, Vitamin D, milk consumption and hip fractures: a prospective study among postmenopausal women. American Journal of Clinical Nutrition, Feb; 77(2), 504-11.
Holick, M. (2005). The Vitamin D epidemic and its health consequences. Journal of Nutrition, Nov; 135(11), 2739S-2748S.